Rule put in place in 2020 prevented state from dropping Medicaid health insurance for enrollees; Millions of Texans will soon have to re-enroll for coverage
Researchers say state preparation, outreach, and navigation to other health insurance options could help minimize a dramatic rise in uninsured
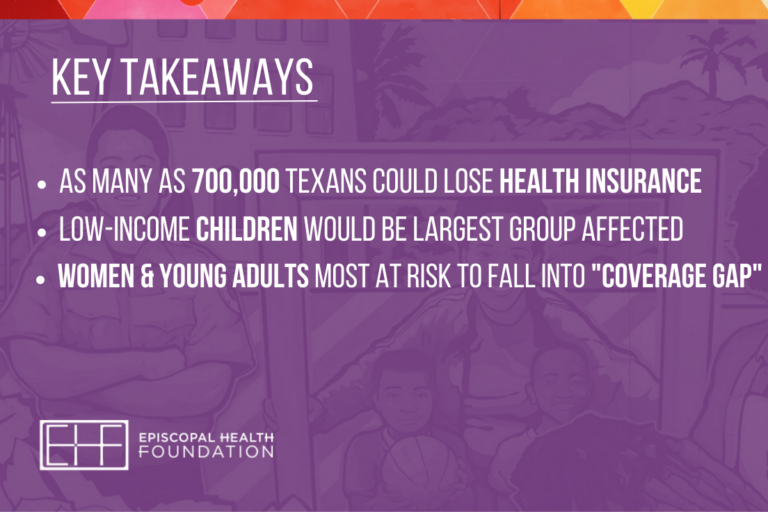
As many as 700,000 Texans could lose their health insurance when a pandemic-related Medicaid rule ends in April, and a majority of those potentially becoming uninsured would be children. Those are some of the findings of a new report from researchers at Texas A&M University that was sponsored by Episcopal Health Foundation.
The report finds that more than 1.6 million additional Texans joined the state’s Medicaid health insurance program during COVID-19, raising total enrollment to more than 5 million. Enrollees are primarily low-income children, pregnant women, and parents of dependent children. Researchers say the more than 40% jump in enrollment was the result of a federal public health emergency (PHE) rule put in place in 2020 that kept the state from dropping Medicaid coverage for all enrollees and exempted them from completing what used to be routine renewal paperwork based on eligibility and income.
The PHE rule is now set to expire in April and the report warns that unless action is taken, conservative estimates show that anywhere from 550,000 to 700,000 Texans would lose their Medicaid health insurance coverage.
“Children would be the largest group potentially to lose health insurance,” said researcher Laura Dague, an associate professor of public service and administration at The Bush School of Government and Public Service at Texas A&M and a Mosbacher Research Fellow. “While the majority of enrolled children will still be eligible for coverage, the potential for large-scale loss of coverage exists because of confusion around the redetermination process including issues like address changes or paperwork mistakes.”
In addition, Dague says large numbers of other enrollees will now be ineligible for Medicaid health insurance under reinstated rules in Texas. For example, children could lose coverage because their parents now earn more than $2,500 a month for a family of three. Low-income pregnant moms who had children in 2020 or 2021 would lose Medicaid insurance because once they’ve given birth, they’re only eligible for continued coverage if they earn less than $251 a month for a family of three.
“Many who lose health insurance won’t know what to do next if they don’t have guidance of what other options exist,” said Dr. Ann Barnes, president and CEO of the Episcopal Health Foundation. “There needs to be increased awareness of how the end of this public health emergency could contribute to the health insurance coverage gap in Texas.”
Texans who will no longer be eligible for Medicaid insurance may have other health insurance options available, including CHIP for children in families who saw modest increases in their income and low or no-cost insurance through the Affordable Care Act (ACA) on HealthCare.Gov for some adults.
Despite those options, researchers say many women and young adults may fall into the health insurance “coverage gap” created when Texas declined to expand Medicaid under the ACA. That gap exists when Texans’ incomes are too high for Medicaid, but too low to qualify for a federal subsidy to buy ACA health insurance.
The report outlines policies and administrative actions that would help maintain the gains in health insurance coverage including:
· Reducing red-tape costs of processing renewals and redeterminations by streamlining eligibility systems
· Including the use of information already available to the state
· Using the capacity of managed care and health insurance navigator organizations for outreach and processing
· Taking advantage of increase federal funding through Medicaid expansion
The healthcare advocacy group Cover Texas Now says Texans who have Medicaid insurance and may still be eligible should update their mailing address with the state by visiting YourTexasBenefits.com, visiting an HHSC benefit office, or calling 2-1-1. Enrollees must also respond to the renewal notice they receive from the state.
Community organizations are also available to provide Texans with no-cost assistance renewing their health coverage or exploring new options. Texans can visit the state’s Community Partner program website to find a local group.
The report “What Happens to Texans’ Insurance Coverage When Medicaid and Marketplace Pandemic-Era Policies End?” was written by Dague & Ben Ukert, an assistant professor of health policy and management at the Texas A&M University School of Public Health.